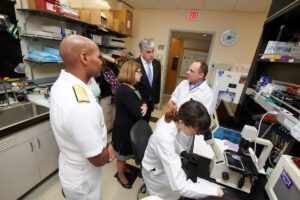
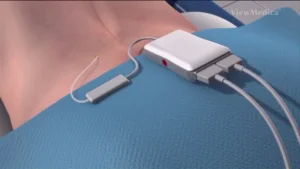
Researchers at Washington University School of Medicine in St. Louis have received a five-year, $11.7 million grant to study human genes and nerve cells to better understand how cells transmit pain and to identify new ways to treat it.
Understanding, treating pain, reducing opioid use, aim of $11.7 million grant (Links to an external site)